How could hospitals possibly keep up with mounting pressure, or tackle increasing staff shortages, when highly educated nurses are still tied up loading trolleys or opening packaging, instead of caring for their patients, or for themselves? Something must change. It’s time to start eliminating non-value added activities in and round the OR, and make room for what truly matters.

9 out of 10 surveyed nurses said that a lack of time had caused them to drop one or more needed care activities on their last shift¹.
Find out where, and how much, resources are normally wasted on non-value added activities before, during and after surgical procedures.

Get ahead and stay efficient. The Mölnlycke OR Efficiency Partnership programme helps you find your flow, evidencing smarter and more efficient ways of working, adding value in the operating room and beyond.

Get an idea of the added value your hospital could gain by switching from your current procedure tray solution to the Mölnlycke OR Efficiency Partnership programme.

Reduce waste and increase efficiency in the operating room with surgical procedure trays. You can customise the sterile packs by including components surgical teams need for specific interventions.

Working more efficiently in the operating room and beyond enables you to reduce the physical waste generated by surgical procedures. But it’s also an effective way to battle burnout and exhaustion of OR staff.
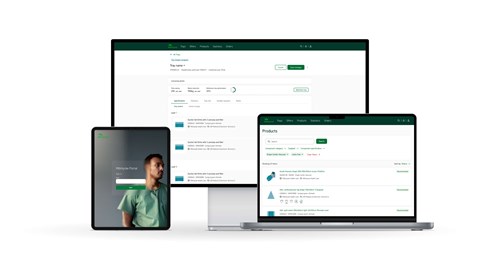
The OR Efficiency Partnership includes a set of highly accessible digital tools that enable you to do everything from customising your ProcedurePak® trays and calculating CO2e savings to tracking and evaluating the efficiency measures you have implemented.
Get started today
Let’s eliminate non-value-added activities and make room for what matters. Reach out to our Mölnlycke representative today to learn what your hospital could gain from the Mölnlycke OR Efficiency Partnership programme and how to get started.
We will handle any privacy data in accordance with our privacy policy (available under Policies).
References
- Ref: Ball JE, Murrells T, Rafferty AM, et al. ‘Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf [Internet]. 2014 Feb 1;23(2):116–25. Available from: https://qualitysafety.bmj.com/content/23/2/116






